What did you do during pregnancy to promote a healthy pregnancy and birth?
Find details on a lot of what I did in this blog post. Most of the things that I describe doing to flip our breech baby were things that I did anyways to prepare for birth- just ramped them up during that time! Maya abdominal massage, chiropractic care, holistic pelvic care and prenatal yoga to prepare physically. This isn’t just about being strong and prepared for labor, but also helps get the uterus into optimal positioning. Hypnobirthing course/meditations, acupuncture, reading and listening to natural birth stories, making a birth plan and having a doula also helped tremendously!
What tips do you have for staying comfortable in the third trimester?
Get a body pillow- I liked using a U-shaped one! Also, get a yoga ball! I sat on it all the time while pregnant used one during birth and still use it to calm Harper and bounce him to sleep. I also did hypnobirthing meditation daily, prenatal yoga, went on walks and did the miles circuit towards the end.
Do you have your birth story on your blog?
Yes! You can read about How Our Breech Baby Flipped at 37 Weeks and our Unmedicated Natural Hospital Birth in these blog posts.
What are your postpartum recovery must haves?
I am SO glad that I had some mamas give me these items because I would have had no idea what I needed! A perineal washer for keeping clean, perineal spray for pain relief, belly wrap for core/back support, herbs and epsom salt for sitz baths, body oil for dry skin and self-care massage, nipple cream for painful breastfeeding/pumping (if you need this there may be an issue please consult an IBCLC). My biggest “must-have” is being prepared mentally as much as possible… read my 8 Mistakes to Avoid During Postpartum here.
What are some ideas for postpartum easy meals?
The easiest meals during postpartum were the ones that I prepped in advance, froze and could reheat. These got eaten up so much quicker than I anticipated and wish I had made even more! You can find the ways I stocked my freezer in this blog post. My other go-tos have been rice bowls or toasts with the goal of packing as much calories and nutrition into one meal as possible! It was key during both pregnancy and postpartum to keep my fridge stocked with the essentials for quick snacks and meals. There is nothing worse than opening an empty fridge when you are 9 months pregnant or a few days postpartum, tired and hangry! Find all my essentials for stocking the fridge in my Pregnancy + Postpartum Nutrition Plan.
What were you told about working out postpartum?
I was cleared to work out by my regular OB at my 6 week check up. However, I knew from my doulas and other mamas that I needed to be careful with this. My holistic OB cleared me for gentle yoga/walking at 6 weeks, low impact cardio at 2 months and high impact workouts at 6 months. I also did physical therapy with a practice that specializes in postpartum care (was covered by insurance) to heal my diastatis recti and strengthen my pelvic floor.
Do you have a sleep schedule? What do you do for sleep/naps?
We don’t have a schedule but we have routines. I like being flexible and try to offer naps and feedings on demand when he cues. We did the Taking Cara Babies newborn class and 4-5 month guide, and I have also used her blog posts to learn about infant sleep. I had no idea developmentally what amounts of sleep infants need or what to do to help him sleep. I hate hearing him cry and am not personally comfortable doing sleep training but also lack of sleep has really taken a toll on my mental and physical health. Her resources have helped me know about how many hours are developmentally appropriate to go between naps, how to look out for sleepy cues and things to do to help him fall asleep and learn to fall asleep. I don’t do all of the stuff she suggests but a lot of it really helped! Sleep is unpredictable like most things in baby world, so I try to let go of expectations and just do what works for us.
How did you discover your sons tongue tie? Did you get it fixed?
The pediatrician at the hospital told us his tongue was “tight”. I didn’t know what that meant and when I followed up with healthcare professionals we were seeing nobody seemed worried about it. Fast forward 3 months and he had fallen off the growth chart and was diagnosed failure to thrive. I brought it up again at that point to one of our healthcare professionals who finally thought it could be the issue. She referred us to a pediatric dentist who diagnosed and revised the ties (both lips and tongue) with a laser that same day. Without getting into two much detail, I highly recommend being evaluated by either a pediatric dentist or ENT as soon as you suspect an issue. Chiropractic care, physical therapy and craniosacral therapy were essential to our recovery process and something we were not referred to but needed to have been. This website helped me learn more about tongue and lip ties after we went through it, but I wish I would have found it sooner.
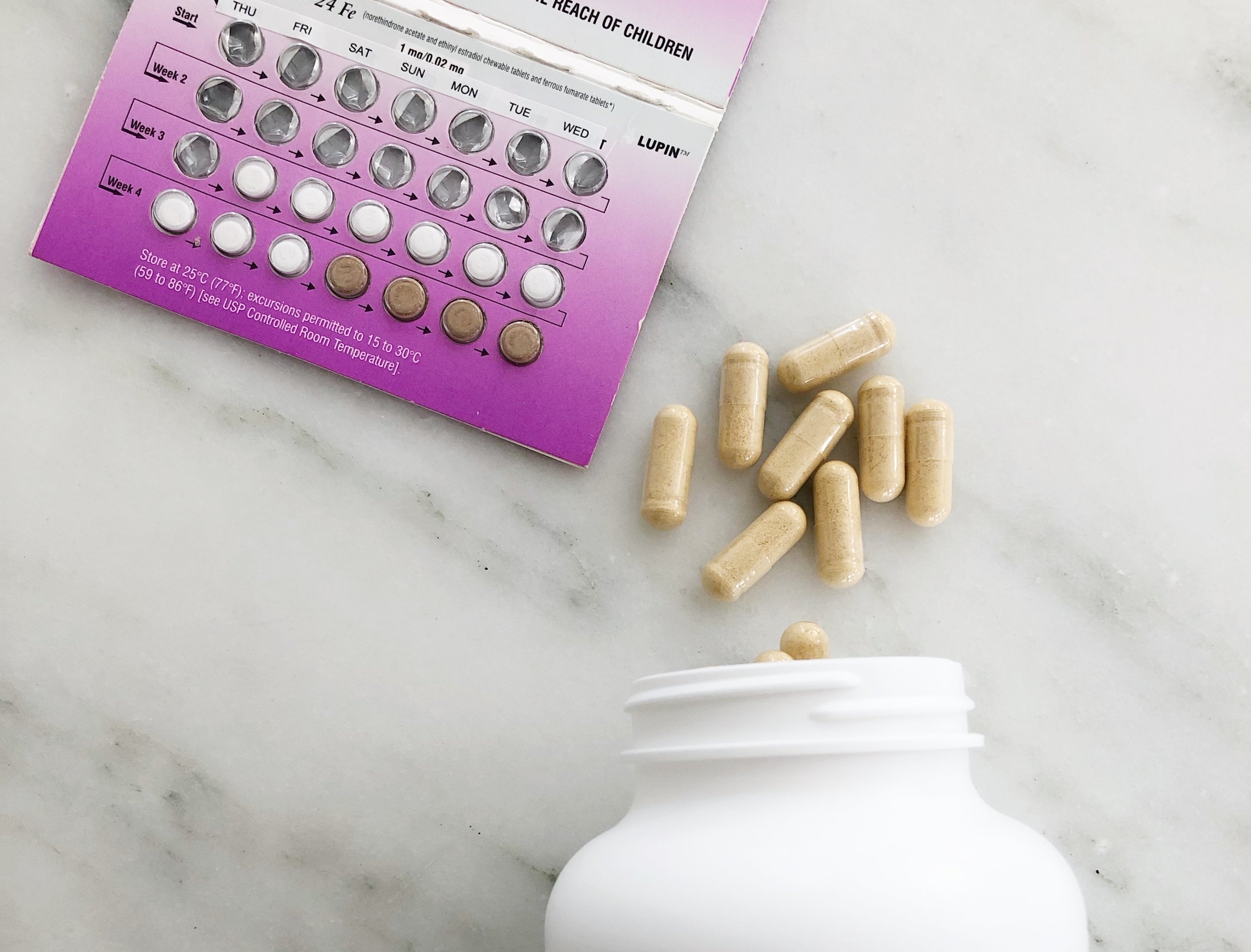
What did you do to increase your milk supply? Did you use supplements?
When I went from nursing a baby with a tongue and lip to to exclusively pumping, I noticed that I did not make as much milk as I thought I did and needed. I was able to quickly amp up my supply with these tips, but please understand that many women’s bodies are not physically able to create all of the milk their babies need. This is nothing to feel guilty or shameful about. It is more common than people think and if you have tried everything under the sun, please know that you are not alone or doing anything wrong.
I would strongly CAUTION against using herbs/supplements. They can sometimes have an adverse effect on both mom and baby. I increased supply mainly with demand. The more your breasts are stimulated either through nursing or pumping, the more demand you create. Nutrition and making sure I was both hydrated (lots of coconut water!) and eating enough nutrient dense foods and calories also helped.
Please also know that breastfeeding does not have to be all or nothing. I made myself crazy exclusively nursing a baby with a tongue and lip tie and then exclusively pumping and trying to latch him 8-12 times a day in addition to bottle feeding him while re-learning to suck. I don’t regret my journey, but now that I have introduced some formula I realize that formula can really help to extend breastfeeding if exclusively breastfeeding is physically or mentally causing distress. Both breast milk and/or formula have everything a baby needs to be healthy, happy and strong.
How do you wash your pump parts?
When I was pumping 8-12 times a day I did the “fridge hack”. This is when you put your parts in the fridge between sessions. I would only refrigerate once so I would use them for 2 sessions. Once I started spacing out my pumping more, I stopped doing the fridge hack. I also got scared when I found out that the CDC warns against it. Now I wash all parts between uses except for the back flow protectors which I wash once a day. During travel, I bring multiple sets in gallon ziplocks and only use them once, then put them in a dirty parts bag to wash at my destination. I bring these wipes in case of an emergency like I forget a part or have to pump at extra time.
How do you travel with breast milk?
I could not figure this out for the longest time and racked my brain for months before traveling! I am sooo happy with both the plans of what we did when traveling with and without Harper.
For traveling with him (this plan is based on exclusively pumping): we bring a days worth of frozen milk and several fresh bottles. I feed the fresh bottles while traveling then serve the frozen milk once it has thawed when we arrive. Why? I don’t want the pressure of pumping and serving immediately during travel thats too stressful so I save that milk and deal with it upon arrival. Since I brought a days worth of frozen milk, I freeze the extra fresh milk I pump on the trip when I get home, This also helps rotate my freezer stash to use up old milk and replace with new. If you do not have a freezer stash, I would bring enough fresh milk to last for the travels if you can and if you are a just-enougher, I would pump directly into the bottles your baby eats from using an adaptor if necessary! ** I haven’t traveled since starting to combo feed and introduce formula so don’t have any tips on that yet!
For traveling without him: I used Milk Stork and it was soooo worth it! I pumped on planes, cars, airports, etc. because I will not waste a drop I just can’t mentally handle that! If you are traveling for work, you can submit a request for your employer to pay for Milk Stork.
Read next…






























Sharing the real, unfiltered details of our sweet rainbow baby after two losses, Graham Nathaniel’s debut! My goal in sharing is to normalize the process of birth and inspire others to feel empowered during pregnancy and birth. There are many reasons people may wish to utilize alternative pain management techniques in birth. The big one for me is that I wanted to go through the physiological birth process. Remember that there is no right or wrong, good or bad in birth as long as the birthing person’s wishes are honored and respected.